- Fertility preservation
- Female cycle & fertility
- Blogs
- Support
Developed in collaboration with Dr Mathilde Bourdon, a fertility specialist from France
We’re often told that women have a ‘ticking clock’ when it comes to their fertility. Is this true?
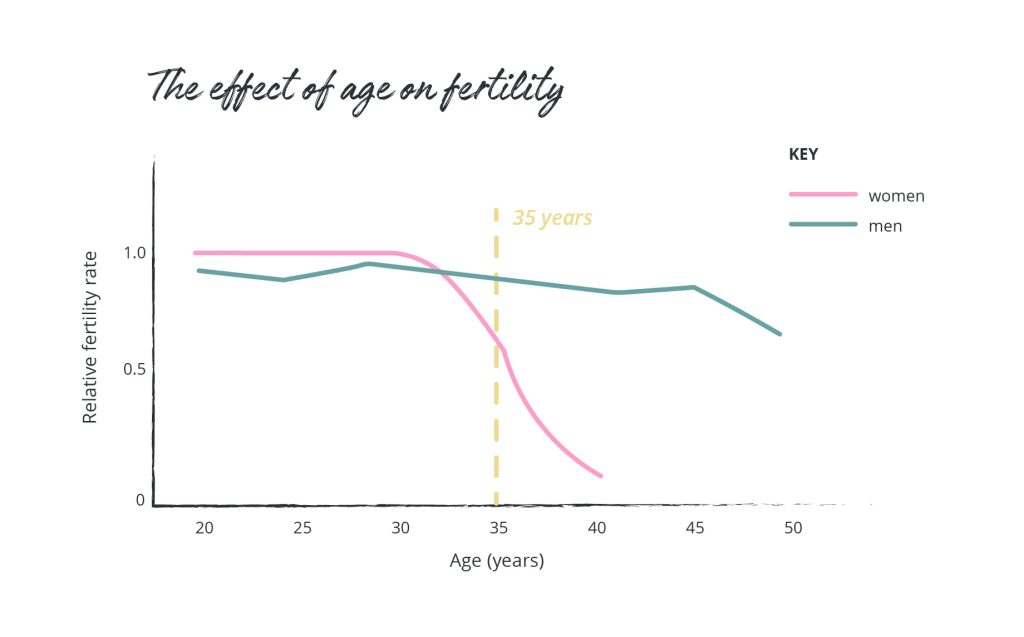
The evidence shows that yes, this is true. Women’s fertility starts to decline gradually after the age of 30, with a steep decline after 35, as both the quantity and quality of our eggs decreases as we get older. And what this means is, if you want to have children after 30, and especially after 35, your chances of conceiving and having a healthy pregnancy are lower than if you tried to have children in your 20s.
So what can we do about it? One of the options for preserving your fertility is egg freezing, which is a process where your eggs are frozen at a younger age so they can be used later in life. For example, if you froze your eggs at the age of 30, and struggled to get pregnant a few years later, you would have a store of eggs that were ‘aged 30’ that you could use to try to get pregnant through IVF. Overall, egg freezing can help to increase your chances of having a healthy pregnancy in the future, but it’s important to know that it doesn’t guarantee pregnancy.
Many people choose to freeze their eggs for different reasons. Some women choose to focus on their career or education, or want more time to meet the right partner, or simply want to reduce the pressure and give themselves more time and options. Whatever your reason, it’s a very personal decision.
The decision tree below is designed to help you start thinking about whether egg freezing might be right for you. It’s not medical advice and only considers your age, not your personal medical history or any underlying health conditions. Some medical conditions can also affect fertility; you can learn more here.
If you’re ever unsure, the best next step is to talk to a doctor or fertility specialist who can guide you based on your individual situation.
This decision tree is a starting point, not medical advice. Everyone’s fertility journey is unique, and it’s always worth getting personalised guidance from a doctor.
If you’re thinking about trying for a baby soon, consider pre-conception counselling and a gynaecological check-up to make sure everything’s on track.
If you’d like to learn more about egg freezing or discuss whether it could be right for you, talk to a fertility specialist — you can download our conversation guide to help you prepare for your first consultation.
Or, if you’re not ready to make any decisions yet, it’s always a good time to learn about your fertility so you can make informed choices in the future. Try our fertility age calculator to better understand your fertility and how it changes over time.
Fertility often feels like something you only need to worry about when you’re ready to start a family. The truth is, understanding your fertility earlier in life gives you the power to make informed choices about your future. Whether you plan to have children or not, it’s helpful to know that your fertility changes as you get older, and can also be influenced by lifestyle and health conditions.
Accessible, inclusive, and accurate fertility education isn’t just for people trying to conceive, it’s something that benefits everyone. When you understand how your fertility works and what affects it, you’re better equipped to make confident, informed decisions that align with your goals, whatever they may be.
Fertility touches almost every part of life, from family and career planning to decisions about health and relationships. But too often, we only start learning about fertility when something isn’t going according to plan.
A lack of knowledge can lead to missed opportunities or misconceptions. For example, many women assume that as long as they’re healthy, getting pregnant won’t be difficult, and that they can rely on IVF if needed. But while IVF works for some people, it’s not guaranteed to succeed, and using lower-quality eggs or sperm reduces the chances of success.
Imagine this: a woman in her late 30s starts trying for a baby, only to find out her ovarian reserve (the number of eggs she has) is lower than expected. She might wish she’d learned about what affects fertility earlier, so she could have made lifestyle changes, been aware of health conditions that impact fertility, or considered options like egg freezing.
Fertility knowledge is power. It allows you to plan, prepare, and feel more in control of your reproductive health instead of being caught off guard.

Despite how important fertility is, it’s not something we talk about much. For many of us, our first formal education about reproduction (if we get any) comes through “sex ed” at school, and even then, the focus is usually on avoiding pregnancy and preventing sexually transmitted infections (STIs). Fertility, when mentioned, is rarely framed as something to understand and take care of throughout life.
This can lead to an unbalanced view: young people grow up knowing how not to get pregnant, but not understanding how pregnancy happens, what affects fertility, or that fertility declines with age for both women and men (with a sharp decline after 35 for women).
As adults, things don’t get much better. Public information about fertility is limited, and conversations about it can feel awkward or taboo. In many cultures, topics like reproductive health and infertility are still seen as private or even shameful. These barriers can make it harder for people to ask questions, seek support, or learn about their options until they face challenges first-hand.
Better education in schools, workplaces, and communities can help break down these barriers. When fertility becomes a normal part of health conversations, it opens the door for empathy, support, and informed decision-making at every stage of life.
Fertility education should be for everyone. That means information that’s clear, non-judgmental, and inclusive of diverse experiences, whether you’re single, in a same-sex relationship, living with a health condition, or you’re not sure if you want children. Understanding fertility isn’t just about women’s bodies, either. Men’s reproductive health plays an equally important role, yet is discussed even less.
Accessible resources help everyone — partners, friends, and families — understand and support each other’s fertility journeys.

If you’re ready to start learning, choose trustworthy sources. Evidence-based educational websites like Fertility Choices, your doctor, and public health organisations are excellent places to start.
AI tools like ChatGPT-5 or Copilot can also be useful for quick overviews or answering specific questions. They’re great for exploring topics in your own time, but they shouldn’t replace expert advice. Always double-check advice with reliable sources and discuss important decisions with your doctor. Your doctor should always be your most trusted source of information.
Knowledge really is power, especially when it comes to fertility. The more you understand about your reproductive health, the more confident and prepared you’ll feel to make decisions that fit your life, your goals, and your body.
Be proactive: start learning about fertility today. Talk about it with your loved ones. Bring it up at your next doctor’s appointment. And if you’re curious about where your fertility might stand right now, try our Fertility Age Calculator to take the first step toward understanding your body better. Your future self will thank you for it.
Making the decision to learn more about your fertility can feel incredibly empowering and nerve-wracking at the same time. Whether you’re actively trying to conceive or simply planning for the future, fertility assessments can offer helpful insights into your reproductive health.
In this blog, we’ll break down what female fertility assessments involve, why you might want to take them, and where to go for them. While we’re focusing on assessments for women here, it’s worth noting that male fertility assessments are just as important.
Fertility assessments are medical checks that help evaluate your reproductive health, normally carried out by a fertility specialist or an obstetrician-gynaecologist (OB/GYN).
Common reasons for fertility assessments:
FAQ: Should I consider testing my fertility even if I’m not trying to get pregnant?
Yes, especially if you’re thinking about having children one day. It can be helpful to get a snapshot of your fertility and plan ahead.
If you’re considering egg freezing, fertility assessments can:
FAQ: What’s the best age to check fertility?
There's no one-size-fits-all answer, but many people choose to test in their early 30s. That said, if you're in your 20s and curious, especially if you're considering egg freezing, there’s no harm in checking sooner.
If you’re planning to talk to a fertility specialist about fertility assessments, it’s important to also ask them about how different fertility treatment options are reimbursed in your country, so you can understand what your options look like at this stage.
Fertility assessments typically include blood tests and other tests like an ultrasound. Depending on your situation, your doctor may also recommend additional tests.
Hormone blood tests:
FAQ: Is AMH reliable?
AMH gives a useful estimate of the activity in your ovaries but doesn't tell you your exact egg count or the quality of your eggs, and it can’t predict when you’ll hit menopause. It’s one piece of the puzzle, not the full picture.
Other assessments:

If you’re interested in fertility assessments, you’ve got a few options:
If you decide to take fertility assessments, it’s important to remember that while they can offer valuable insights into your reproductive health, they can’t provide certainty. A normal result doesn’t guarantee you’ll conceive easily, and a low ovarian reserve doesn’t mean pregnancy is impossible – this is why it’s best to ask your doctor for advice when you assess your fertility health.
It’s also important to acknowledge that fertility assessments can be emotional. They might bring up difficult feelings, or spark tough conversations with your partner or family. That’s completely normal. If you need support with having difficult conversations with your loved ones, our guides are here to help.
Fertility assessments won’t give you all the answers, but they can be a helpful first step on your fertility journey. Whether you’re just starting to explore your fertility or you’re currently trying to get pregnant, these assessments can help you to understand your choices and make informed decisions.
If assessing your fertility feels like a big step for now, you can get an idea of how your fertility is expected to change with age by checking our fertility age calculator.
Fertility is influenced by a wide range of factors, some of which you can change, and some you can’t. In Part 1 of this blog, we explored lifestyle and environmental factors that you can influence, such as diet, exercise, and sleep. In this second part, we’ll look at the factors that are outside of your control and explain what you can still do to protect or preserve your fertility.
Age is the most important factor affecting fertility, especially for women.
a) Health Conditions
In women, health conditions that affect fertility may include:

In men, common conditions that affect fertility include:
b) Medications
For women, medications that may impact fertility include:
For men, medications that may impact fertility include:
If you're planning to conceive, it’s important to speak to your doctor about whether your medications could affect your fertility.
c) Genetic Factors
Sometimes, fertility challenges run in families. If close relatives experienced the below conditions, you may be affected by these conditions as well:
While you can’t change your genes, being aware of your family’s medical history can help you make informed decisions earlier.
If you’re thinking about starting a family someday and are worried about how factors like age or health conditions might affect your chances, learning about your options for preserving your fertility is the best first step you can take.
Egg freezing (for women) and sperm freezing (for men) allow you to store your eggs or sperm at a younger age, when the quality is higher. These options don’t guarantee a successful pregnancy later, but they can increase your chances if you face age-related or medical fertility challenges when you start trying for children.
If you have a medical condition or a family history of fertility issues, it’s worth speaking to a fertility specialist to explore your options early.
While you can’t change your age or your genes, understanding how these factors influence fertility can help you to plan ahead. When you combine this knowledge with healthy lifestyle choices (covered in Part 1 of this blog), you give yourself the best possible chance of conceiving when the time is right for you.
Remember: Everyone’s fertility journey is different. If you have questions or concerns, don’t hesitate to talk to your general practitioner or a fertility specialist.
Being informed is the first step. Take a moment to explore our fertility preservation section (at the top of your screen) and start your journey today.
Fertility is a complex process which can be affected by many factors, some of which you can control, and some which you can’t. Knowing how lifestyle and environmental factors can affect your fertility can help you make simple changes to improve your chances of getting pregnant.
In this blog, we will explore how different factors such as diet, exercise, weight, smoking, alcohol, recreational drugs, stress, sleep, and your job can affect fertility for both women and men.
What we eat plays a crucial role in fertility. A diet rich in antioxidants, vitamins, and minerals supports reproductive health, while processed foods and excessive sugar can negatively impact hormone levels and sperm quality.

Regular physical activity supports hormonal balance and overall health, but too much or too little can have negative effects.
Read more about exercise and fertility here.
Being underweight or overweight can interfere with fertility.
Read more about weight and fertility here.
Poor sleep patterns can disrupt reproductive hormones and reduce fertility.
Aim for 7–9 hours of quality sleep each night and maintain a consistent sleep schedule.
Substances like tobacco, alcohol, and other recreational drugs have a significant negative impact on fertility.
For both women and men, fertility can be improved by quitting smoking, stopping or limiting alcohol intake to moderate levels, or avoiding recreational drugs. Read more about smoking and fertility here.
Chronic stress affects the body’s hormonal balance, which can interfere with ovulation in women and reduce sperm count and quality in men.
Managing stress through relaxation techniques, mindfulness, exercise, and therapy can help regulate hormone levels and improve fertility. If you are feeling stressed at work, there are a lot of helpful tips online to help you create a better work-life balance.
Read more about stress and fertility here.

Conditions in certain jobs can affect fertility.
Read more about work and fertility here.
While some factors that affect fertility are beyond our control, taking small, consistent steps toward a healthier lifestyle may enhance your reproductive health, and you may be able to improve your chances of getting pregnant. However, it’s important to remember that everyone’s fertility journey is unique, and what works for some people may not work for you. Always consult a healthcare professional if you need more guidance.
As part of your fertility journey, it’s also important to think about the things we can’t control, like age and health conditions, as these can impact fertility even more than lifestyle factors. You can read more about this in Part 2 of this blog (coming soon!).
Developed in collaboration with Daniella Corder | Menstrual cycle health & fitness coach (@coach_cords)
If you’ve ever felt amazing during a workout one week but sluggish and unmotivated the next, you’re not imagining things—your menstrual cycle could be playing a big role in how you feel. Hormonal fluctuations throughout the month impact your energy levels, metabolism, and even how your body responds to working out and what you eat.
Instead of pushing through workouts that don’t feel right or battling cravings without understanding why, adapting your approach to align with your cycle can be a game-changer. By working with your body rather than against it, you can improve performance, recovery, and overall wellbeing.

Developed in collaboration with Daniella Corder | Menstrual cycle health & fitness coach (@coach_cords)



If you’ve ever felt amazing during a workout one week but sluggish and unmotivated the next, you’re not imagining things—your menstrual cycle could be playing a big role in how you feel. Hormonal fluctuations throughout the month impact your energy levels, metabolism, and even how your body responds to working out and what you eat.
Instead of pushing through workouts that don’t feel right or battling cravings without understanding why, adapting your approach to align with your cycle can be a game-changer. By working with your body rather than against it, you can improve performance, recovery, and overall wellbeing.
Your menstrual cycle isn’t just about your period, it’s a month-long process that affects everything from your mood to your metabolism. It consists of four phases: the menstrual phase (days 1–4), the follicular phase (days 5–17), ovulation (around day 17), and the luteal phase (days 18–29).


Understanding these phases can help you adjust your workouts and diet to support your body’s natural rhythms rather than working against them.
As hormonal fluctuations throughout the menstrual cycle can impact energy and performance, there are simple way to adjust your workouts to maximise your potential in each phase.




Fasted training (working out on an empty stomach) is thought to help your body burn fat faster, as there is less sugar readily available in your body from food.
While this approach to training is popular, research has shown that fasted training may not be suitable for women as our brains are more sensitive to a low availability of energy than men’s. As a result of this, when we don’t provide enough energy to our body before a workout (e.g. if we train fasted), we are more likely to use our muscle tissue as fuel because our body will try to maintain our fat and carbohydrate stores.
For women, the recommended amount of food before working out is:
• 15 g of protein for strength-based workouts, OR
• 15 g of protein AND 30 g of carbohydrate for strength and cardio-based workouts
Of course, remember that all bodies are different, and if you struggle to eat a lot before your workouts, try a light pre-workout snack that is high in protein and carbohydrates, such as a small protein shake and a banana.
Just like your workouts, your diet should align with your cycle to optimise energy and recovery.
Your menstrual cycle is a powerful tool, not a barrier, to feeling your best. By adapting your workouts and diet to match your body’s natural rhythms, you can improve performance, reduce fatigue, and support your overall health.
Start by making small changes, such as tracking your cycle and scheduling reminders in your calendar to help you remember to adjust your workouts and diet as you enter each phase of your menstrual cycle. For example, you could set reminders to focus intense workouts during your follicular phase or to add more magnesium-rich foods to your diet in your luteal phase. Over time, you’ll find a routine that works for you, embracing your cycle rather than fighting against it.
So, next time you feel off during a workout or find yourself craving carbs, remember: your body isn’t working against you, it’s trying to tell you what it needs. The more you listen, the better you’ll feel.